Find experienced and well trained Hand Surgeons across the UK
Metacarpalphalangeal Joint (MCJP) Arthroplasty
Traditionally MCPJ replacements have been of silicone construction inserted into patients with rheumatoid disease. However osteoarthritis (OA) either primary or secondary to trauma does occur. In these patients it has been shown that a more stable MCPJ replacement such as the Ascension Pyrocarbon type is more suited.
Rehabilitation for RA and OA is very different:
Post Operative Hand Therapy for RA:
Two protocols are available: -
- Dynamic Regime
- Static regime
The DYNAMIC REGIME is the preferred protocol, but the STATIC REGIME should be considered when there are justifiable circumstances.
Aims of treatment:
Improve function by:
- Correcting deformity
- Relieve pain
- Altering arc of flexion / extension (most commonly it is extension that requires the greatest increase in movement but achieving this must not be at the expense of functional flexion).
- Improved cosmesis is frequently achieved by this procedure and maintaining this is important to many individuals.
Immediate Post-operative Period:
- Elevation
- Antibiotics
- Pain relief
Day 2:
- Removal of post-op dressing
- Wound inspection
- Removal of silastic drain
- Reapplication of volar supporting splint (post op POP if comfortable or custom made thermoplastic resting splint, see appendix 1)
Day 3-5:
- Elevation of hand
- Pain relief as appropriate
- The patient may be discharged from hospital at this point if medical and social circumstances permit.
Day 5 Dynamic Regime:
- If Outpatient re-admit to ward for over night stay or as day patient dependent on medical & social circumstances and distance from hospital.
- Construction / Application of Outrigger / Commencement of exercise regime (see appendix 2&3)
- Review / Application of Night Resting Splint
Day 6:
- Review of outrigger and exercises as Inpatient or Outpatient.
- ADL needs attended to in preparation for discharge.
- If Inpatient normally patient is discharged home depending on medical & social circumstances.
- Check patient follow-up details and arrange Therapy follow up as appropriate.
Day 14:
- Removal of sutures in Outpatient
- Review of skin condition
- Review of Outrigger and Night resting Splint efficiency and comfort
- Review of exercise programme and Range of Movement
Follow Up weeks 2-6:
- Minimum weekly attendance in Therapy Department to ensure maximum efficiency of splints and patient exercise regime.
- Scar care as appropriate
- Introduction of additional exercises to increase flexion or extension or both.
- Introduction of static flexor / extensor splints as appropriate.
- Check patients follow up details and arrange Therapy follow-up as appropriate
Week 6:
- Reviewed either in Outpatient Department by consultant.
- If joints stable and good correction of ulnar deviation has been maintained cease the use of Outrigger splint
- If there is poor correction of ulnar deviation and /or laxity of the joints the Outrigger can be retained for a further 2 weeks.
- If the patient exercises more efficiently against the rubber band and resistance provided by the Outrigger the splint can be retained for a further 2 weeks for exercise only.
- Joint protection advice
- Commence light function applying joint protection principles
- Ulnar Deviation protection splinting as appropriate to individual ROM / Deformity / ADL circumstances.
Follow-up Weeks 6-12:
- Patient reviewed in Therapy as frequently as is dictated by the individuals needs.
- Review appointment at 12 weeks for discharge.
- STATIC REGIME This involves the use of 2 static splints. Figure 3
Splint 1
- Wrist extension 30 degrees
- MCPJs flexed, ideally 60-70 degrees
- IPJs extended 0 degrees
Splint 2
- Wrist extension 30 degrees
- MCPJs extended 0 degrees
- IPJs extended 0 degrees
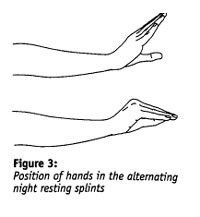
- The splints are alternated every 24 hours.
- Splint removed hourly during the day for active exercise
- Isolated MCP joint flexion
- Isolated IP joint flexion
- Mass flexion
- Passive MCP joint extension
- Active MCP joint extension
- Radial finger walking
This protocol was prepared by: -
Lynda Gwilliam, Clinical Specialist Occupational Therapist, Wrightington Hospital Hand & Upper Limb Therapy. Reviewed with Ann Birch, Clinical Specialist Physiotherapist, Wrightington Hospital Hand & Upper Limb Therapy. August 2006
Appendix 1
Volar based hand/wrist static splint for MCP joint arthroplasties
The initial purpose of this splint is to support the MCP joints in maximum comfortable extension and to maintain the correction of MCP joint ulnar deviation obtained through surgery during the inflammatory phase of wound healing.
Immediately post –op, in theatre, this position is achieved by the application of a volar bases POP slab.
Upon dressing reduction (day 2) this POP slab can be reapplied if effective and comfortable or replaced with a custom made thermoplastic splint, which has the same clinical objectives.
For the first 5 days post-op the splint is worn 24 hours a day to support the MCP joints.
If the patient has retained the post-op POP for the first 5 days it is replaced with a thermoplastic splint on day 5 post-op.
The longer-term purpose of the splint (collagen formation) is to prevent the recurrence of MCP joint ulnar deviation and maintain /increase MCP joint extension during periods of daytime rest and during the night.
Occasionally, at 3 weeks post –op, if extension of the MCP joints is good but flexion poor the splint can be remoulded to encourage flexion of the MCP joints.
The position and efficacy of this splint should be reviewed at each follow-up visit.
To discourage recurrence of pre-operative deformity, and maintain optimal alignment and ROM of the MCP joint arthroplasties, this splint is retained at night during the tissue maturationphase of healing (3-6 months)
Appendix 2
Dynamic Extension Splint (DES or Outrigger)
The purpose of this splint is to: -
- Protect the soft tissue reconstructions performed during surgery.
- Prevent recurrence of pre-operative deformity.
- Assist the relocated weak extensor tendons achieve maximum tissue excursion and movement of the MCP joints.
- Correct any residual deformity.
- Provide “bio feed back” to the flexor mechanisms of the MCP joints to assist with active flexion of the MCP joints.
- Immobilise/stabilise the wrist joint to direct the most efficient flexor power to the MCP joints.
For the majority of patients this will be achieved via a low profile outrigger (if ulnar deviation of the MCP joints is still significant, or the patient has considerable difficulty achieving flexion of the joints a high profile outrigger or alternate regime should be considered).
Because most patients suffering from RA have very fragile skin the base of the splint must be well fitting at all times. This will require frequent monitoring and some alterations as oedema reduces and the arc of movement changes. The tension on the elastic should support the MCP at neutral and allow maximum MCP flexion.
Links:
Evidence:
- I A Trail, J A Martin, D Nuttall, J K Stanley. Journal of Bone & Joint Surgery (British volume)2004 Vol.86,Iss 7. pg.1002. Seventeen-year survivorship analysis of silastic metacarpophalangeal joint replacement
- J Stothard, A E Thompson, D Sherris Journal of Hand Surgery (British volume, 1991) 16B: 61-65. Correction of ulnar drift during silastic metacarpophalangeal joint Arthroplasty
- R. Delaney, I A Trail, D Nuttall. Journal of hand surgery (British and European Volume, 2005) 30B: 1: 3-7. A comparative study of the outcome between the Neuflex and Swanson metacarpophalangeal joint replacements
- H L Kimball, A L Terrono, P Feldon, D S Zelouf. AASO Instructional Course Lectures, Volume 52, 2003. Metacarpophalangeal Joint Arthroplasty in Rheumatoid Arthritis
- N Burr, A Pratt. British Journal of Hand Therapy 1999 Vol 4 No 4. MCP Joint Arthroplasty case Study: The Mount Vernon Static regime
- A Burt. Journal Of Physiotherapy Sept 1986, Vol 72 No 9. Physiotherapy following Joint replacement in the Hand
- N Burr, A L Pratt, P J Smith. Journal of hand Therapy. Philadelphia: Jan-Mar 2002. Vol 15 Iss 1, pg 41. Alternative splinting and rehabilitation protocol for metacarpophalangeal joint Arthroplasty in patients with rheumatoid arthritis
- E T O’Brian. Clinics in Plastic Surgery, Vol 23, No 3, July 1996. Surgical Principles And planning For The Rheumatoid Hand and Wrist
- K Schmidt, R E Willburger, R K Miehlke, K Witt. Scan J Plas Reconstr Hand Surg 33: 433-438, 1999. Ten Year Follow-up of Silicone Arthroplasty of the Metacarpophalangeal Joints in Rheumatoid Hands
- H Ishikawa, A Murasawa, T Hanyu. Journal of hand Surgery (British and European Volume, 2002) 27B: 2: 180-183. The effects of activity and type of rheumatoid arthritis on the flexible implant arthroplasty of the metacarpophalangeal joint
- S G Flemming, E L Hay. The Journal of Hand Surgery. Vol 9-B. October 1984. Metacarpophalangeal Joint Arthroplasty, Eleven Year Follow-up
- A B Swanson, G Swanson, H Ishikwawa. Clinical Orthopeadics and related research Number 342, pp22-33. Use of grommets for flexible implant resection Arthroplasty of the metacarophalangeal joint
- H Gellman, W Stetson, R Brumfield, W Costigan, S Kuschner. Clinical orthopaedics and related research, Number 342, pp 16-21. Silasic metacarpophalangeal joint Arthroplasty in patients with rheumatoid arthritis
- W Ruther, B Verhestraeten, B Fink, K Tillman. The Journal Of hand Surgery Vol 20B No 5 October 1995. Resection Arthroplasty of the metacarpophalangeal joints in rheumatoid arthritis
- M Rittmeister, M Porsch, M Starker, F Kerschbaumer. Arch Orthop Trauma Surg (1999) 119:190-194. Metacarpophalangeal joint Arthroplasty in rheumatoid arthritis: Results of Swanson implants and digital joint operative Arthroplasty
- M Roth. Acorn Journal Vol 60, No 6 1994. Metacarpophalangeal joint implant Arthroplasty
- P A McArthur, R H Milner. Journal of Hand Surgery ( British and European Volume, 1998) 23B: 574-577. A Prospective Randomised Comparison of Sutter and Swanson Silicone Spacers
- K Moller, C Sollerman, M Geijer, P Kopylov, M Tagil. Journal of Hand Surgery (British and European Volume , 2005) 30B: 1: 8-13. Avanta versus swanson silicone implants in the MCP joint- a prospective, randomised comparison of 30 patients followed for 2 years
- J Haber, J A Boswick, D B Phelps. Clinical Orthopeadics and related research, No 140, May 1979. The role of soft tissue reconstruction in flexible implant Arthroplasty of the metacarpophalangeal joint
- W F Blair, D G Shurr, J A Buckwalter. The journal of bone and joint surgery, Vol 66-A No 3, March 1984. Metacarpophalangeal joint implant arthroplasty with a silastic spacer
- T P M Vliet Vlieland, T P van der Wijk, I M M Jolie, A H Zwinderman. The Journal Of Rheumatology1996:23:835-40. Determinants of hand function in patients with rheumatoid arthritis
- S A Emerson. Journal of Hand Therapy July – September 1993Modification of common treatments in hand rehabilitation


